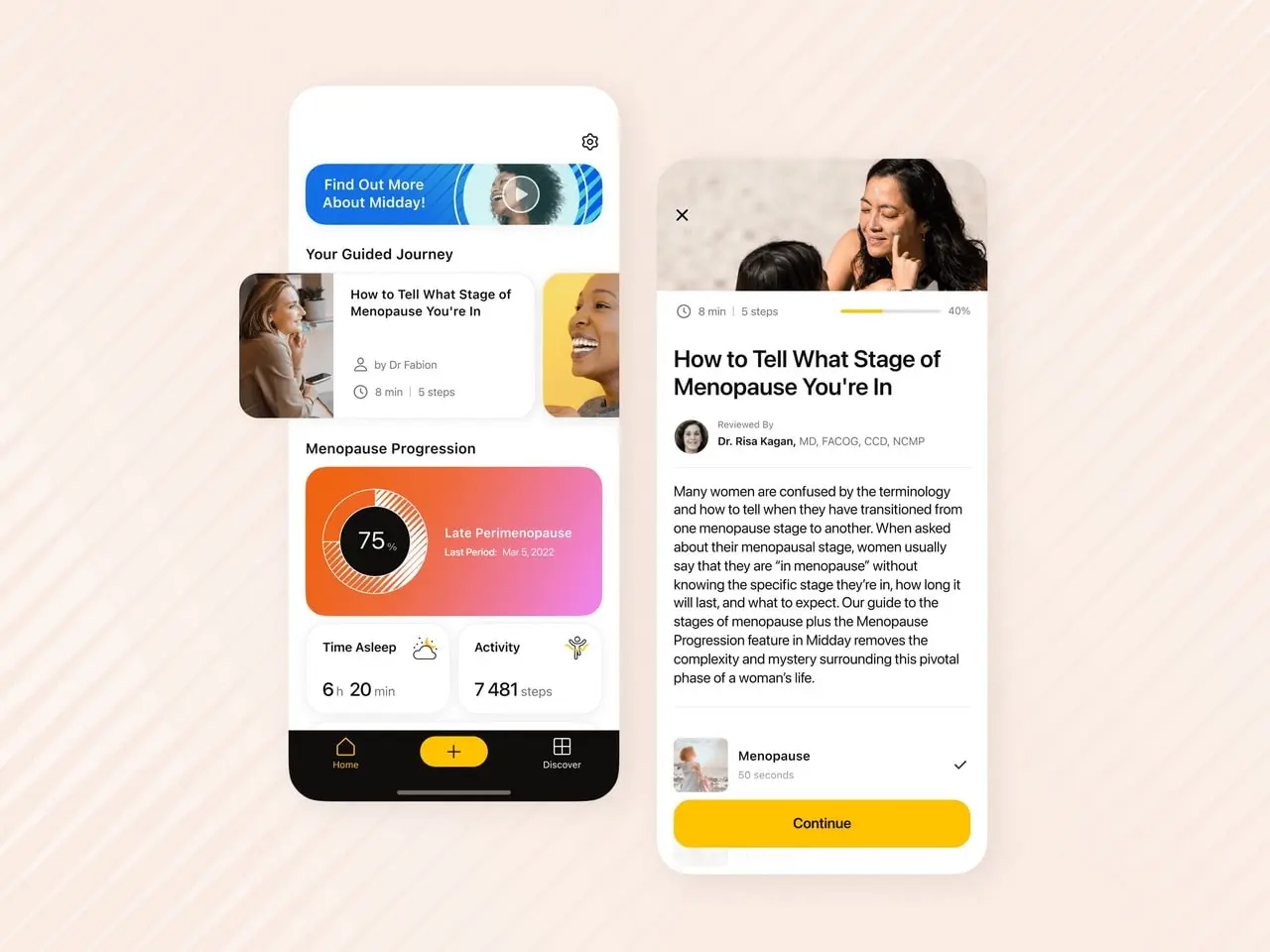
Advanced women's health app that combines a scientific approach with data analytics to help manage menopause symptoms comfortably.
Implementing a Custom EHR in a US Hospital Network: Driving $20 Million in Annual Savings




Emerline developed and implemented a custom EHR solution that enabled one of the largest regional hospital networks in the US to achieve over $20 million in proven annual savings by significantly reducing administrative costs and enhancing operational and clinical efficiency.
Client & Background
Our client is a large, multidisciplinary hospital network in the US, ranking among the top 15 largest in its region by patient volume, with an annual turnover exceeding $5 billion. Its extensive operations span key Midwest states like Ohio, Illinois, and Michigan. The network comprises over 30 hospitals, 150 specialized clinics, and 200 outpatient centers. Daily, they serve tens of thousands of patients, providing a wide range of medical services from primary care to complex surgical procedures.
Historically, the client faced several critical challenges due to outdated systems and manual processes that negatively impacted care quality, operational efficiency, and financial stability:
- Unsuitable off-the-shelf EHR solutions and high TCO risk
Despite attempts to implement standard EHR systems from leading vendors, these proved too rigid and inflexible to adapt to the unique, complex clinical workflows of multidisciplinary teams and various facility types (hospital, specialized clinic, outpatient center).
For example, standard modules couldn't effectively support specific protocols for managing patients with rare oncological diseases or multi-stage cardiac surgeries, requiring excessively expensive and labor-intensive customizations.
Such deep modifications to off-the-shelf systems often invalidated their standard certifications, creating high risks of HIPAA non-compliance with every update. This ultimately made the total cost of ownership (TCO) unacceptably high, with estimated additional annual costs for customizing and supporting third-party EHRs reaching $4-8 million without addressing the client's fundamental needs.
Estimated additional costs for customizing and supporting third-party EHRs could reach $4-8 million annually without yielding the desired results.
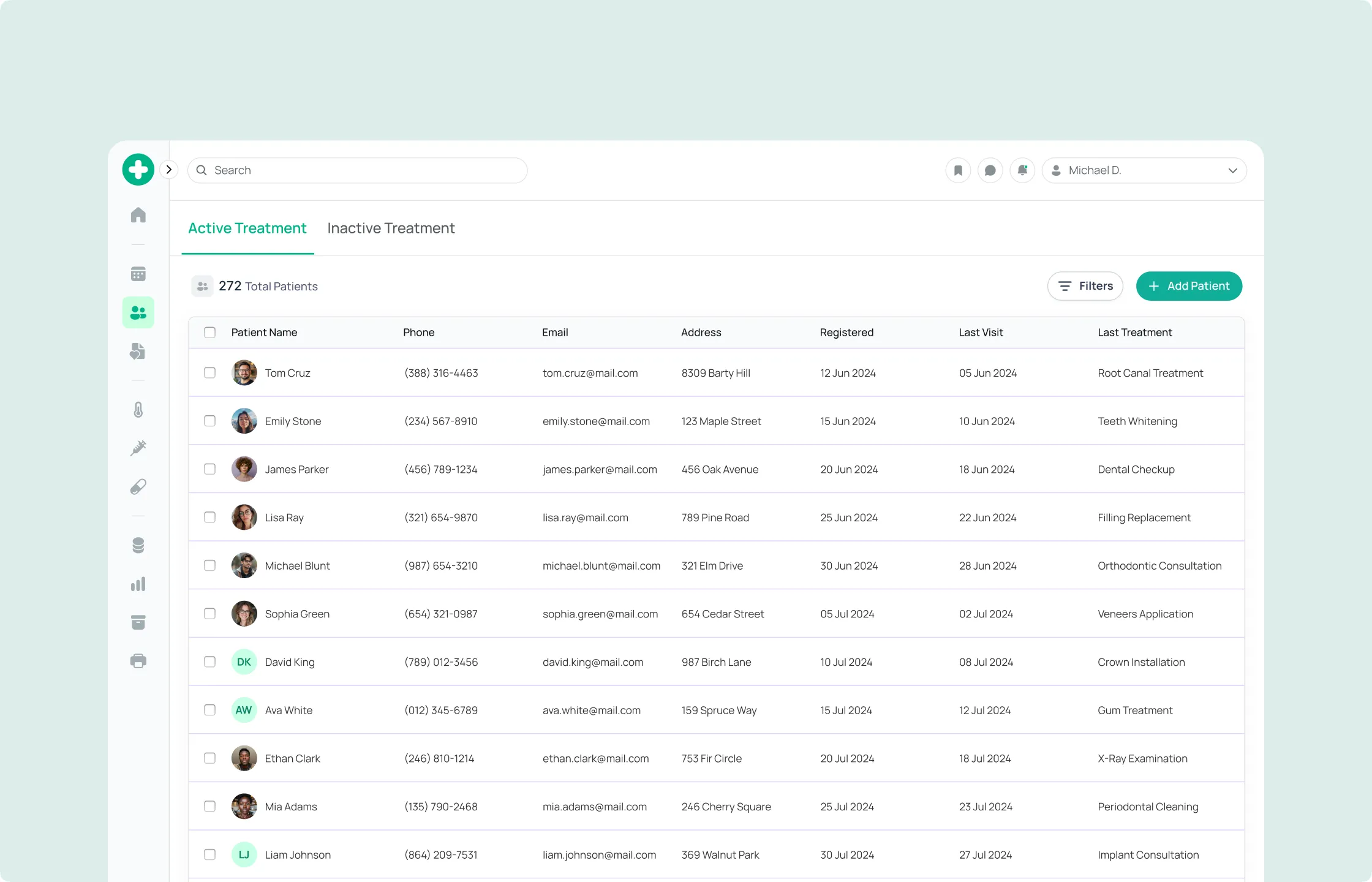
- Fragmented medical records and lack of a unified patient view
Patient information was scattered across numerous disconnected systems: outdated EMRs (Electronic Medical Records) in different hospitals, paper charts in outpatient clinics, and separate systems for labs, radiology, and pharmacies. This led to a lack of a complete and up-to-date overview of a patient's medical history, hindering care coordination and increasing the risk of medical errors.
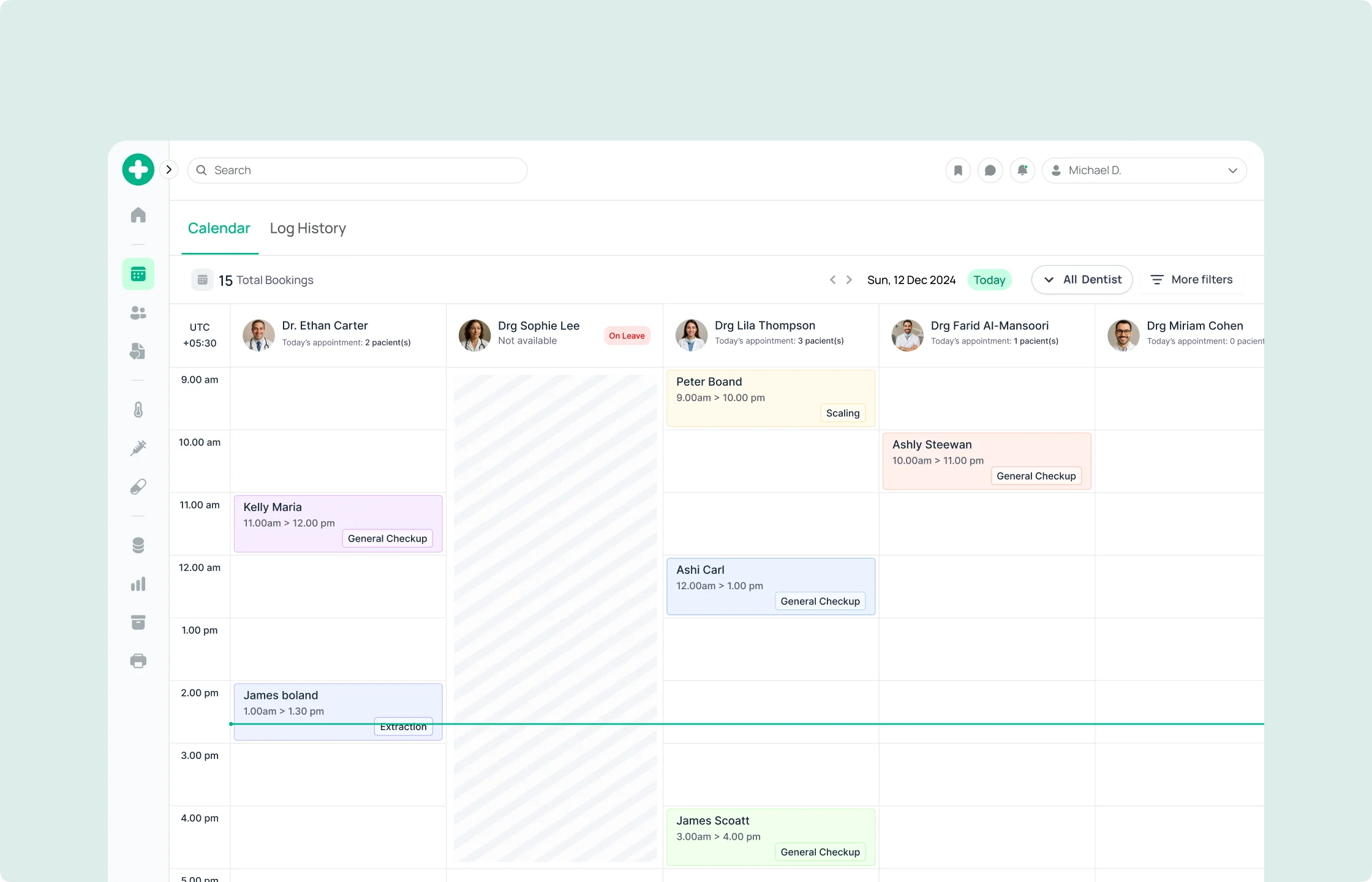
- Low operational efficiency and high administrative burden
Clinical and administrative staff spent an excessive amount of time (up to one-third of their workday) on routine, repetitive tasks: manual data entry, searching for information across different systems, filling out paper forms, and faxing referrals. This reduced productivity, caused staff burnout, and increased operational costs.
- Data security threats and HIPAA compliance complexities
Storing sensitive patient data in disparate, often outdated systems created serious vulnerabilities to cyberattacks and unauthorized access. Adhering to stringent US federal and state regulations for patient data protection, such as HIPAA (Health Insurance Portability and Accountability Act), as well as HITECH Act standards, was extremely labor-intensive and carried high risks of multi-million dollar fines for violations. The risk of HIPAA fines reached hundreds of thousands to millions of dollars per incident, not including reputational damage.
- Lack of clinical decision support tools
Physicians lacked quick access to aggregated patient data at the point of care, as well as intelligent tools that could provide up-to-date clinical guidelines, drug interaction alerts, or potential allergy warnings. This increased the likelihood of errors in diagnosis and treatment.
- Patient engagement challenges
Patients lacked convenient access to their medical records, lab results, online appointment scheduling, or secure communication with physicians, which reduced their engagement in the treatment process and overall satisfaction.
Facing the critical challenges outlined above, the client turned to Emerline.
Methodology
Comprehensive analysis of clinical workflows and data security
EHR architecture and clinician UX/UI design
Iterative development and implementation of core modules
Development of clinical decision support systems and secure data exchange
Integration with telemedicine, billing, and patient portal
Deployment, training, and ongoing support/compliance
Challenges and Approaches
- Staff resistance: Personnel were accustomed to old systems and manual processes. We overcame this by conducting intensive training, creating "champions" among the staff who demonstrated the benefits of the new system, and actively soliciting feedback for iterative UI/UX improvements.
- Data migration complexity:Transferring millions of records from disparate legacy systems presented a colossal task. We used automated ETL (Extract, Transform, Load) tools and strict data validation protocols to ensure the integrity and accuracy of migrated information, minimizing operational disruptions.
- Integration with legacy systems:Some specialized medical devices and third-party systems (e.g., older radiology systems) did not support modern protocols. We developed custom adapters and API gateways to ensure seamless data exchange, avoiding costly equipment replacement.
Solution
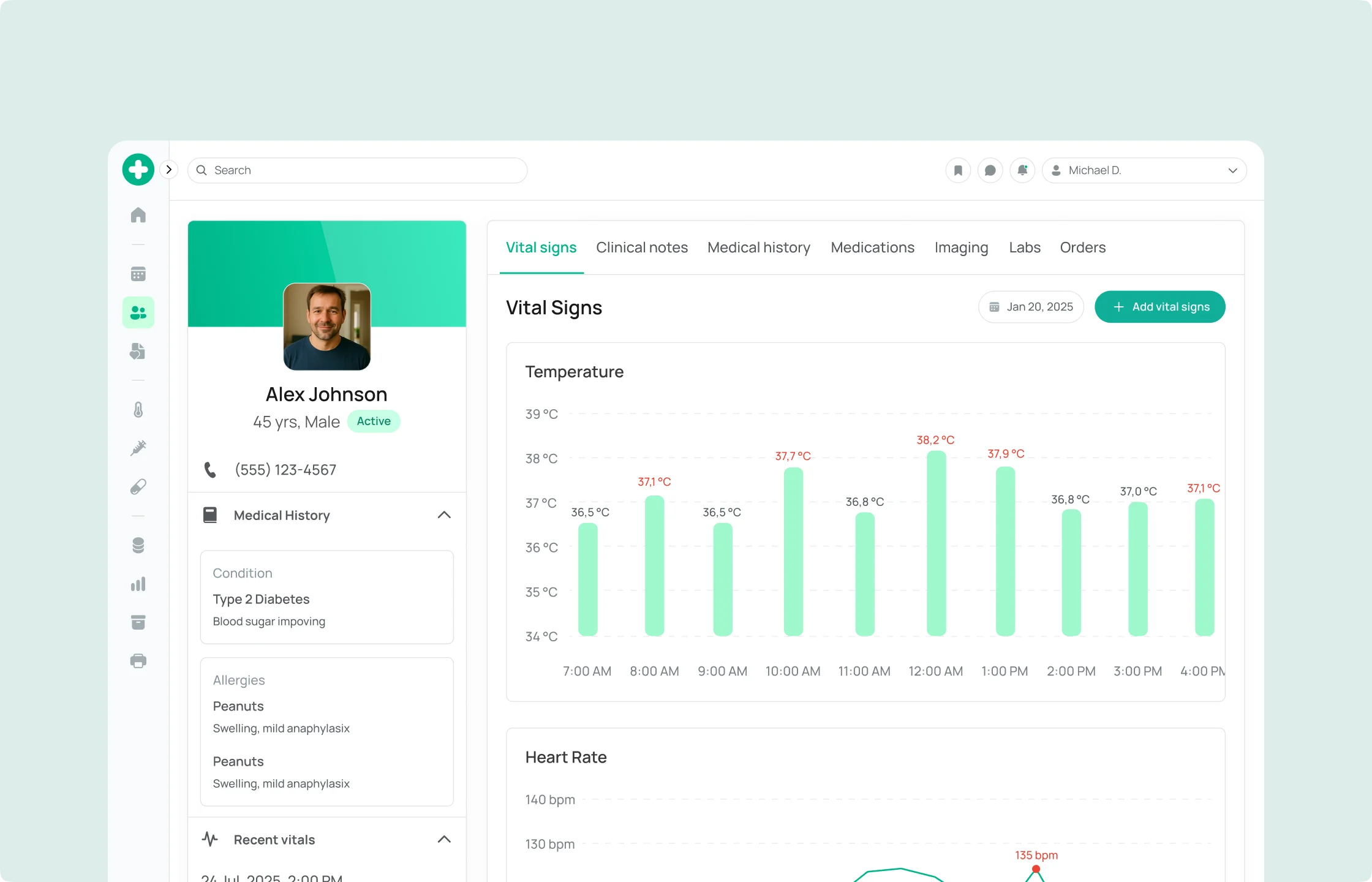
We developed and implemented a custom EHR solution that became a centralized, highly secure, and intelligent platform for patient health management, completely transforming the client's operational and clinical processes.
Our custom EHR surpasses off-the-shelf solutions and typical customizations due to its inherently modular architecture and deep adaptation to the following aspects, providing a unique competitive advantage:
- Specific clinical workflows
We created specialized modules to support complex multidisciplinary consultations, integrate data with high-precision diagnostic equipment (e.g., genetic sequencers or specialized MRIs), and dynamic forms for managing patients with chronic diseases — features impossible to implement in standard systems without radical reworks. This allowed the client to offer unique medical services unavailable to competitors using generic solutions.
- Flexible and intuitive UI/UX
Interfaces were designed considering the individual needs of various specialties (surgeons, internists, nurses), significantly reducing training time and improving usability. This led to faster adoption and higher staff satisfaction compared to implementing generic systems.
- Scalability at the data and functional level
The architecture allows for easy addition of new clinics and specialized centers to the network without rebuilding the entire system, as well as integrating new medical technologies and modules. Since implementation, the client has successfully integrated 3 new clinics into the network, confirming the claimed scalability and saving up to $500,000 on each new connection by leveraging the ready, adapted infrastructure. This ensures the client's long-term investment sustainability and flexibility, allowing them to grow and adapt to future market demands without the need for major IT infrastructure overhauls, a critical distinction from "off-the-shelf" solutions with their update cycles and high TCO.
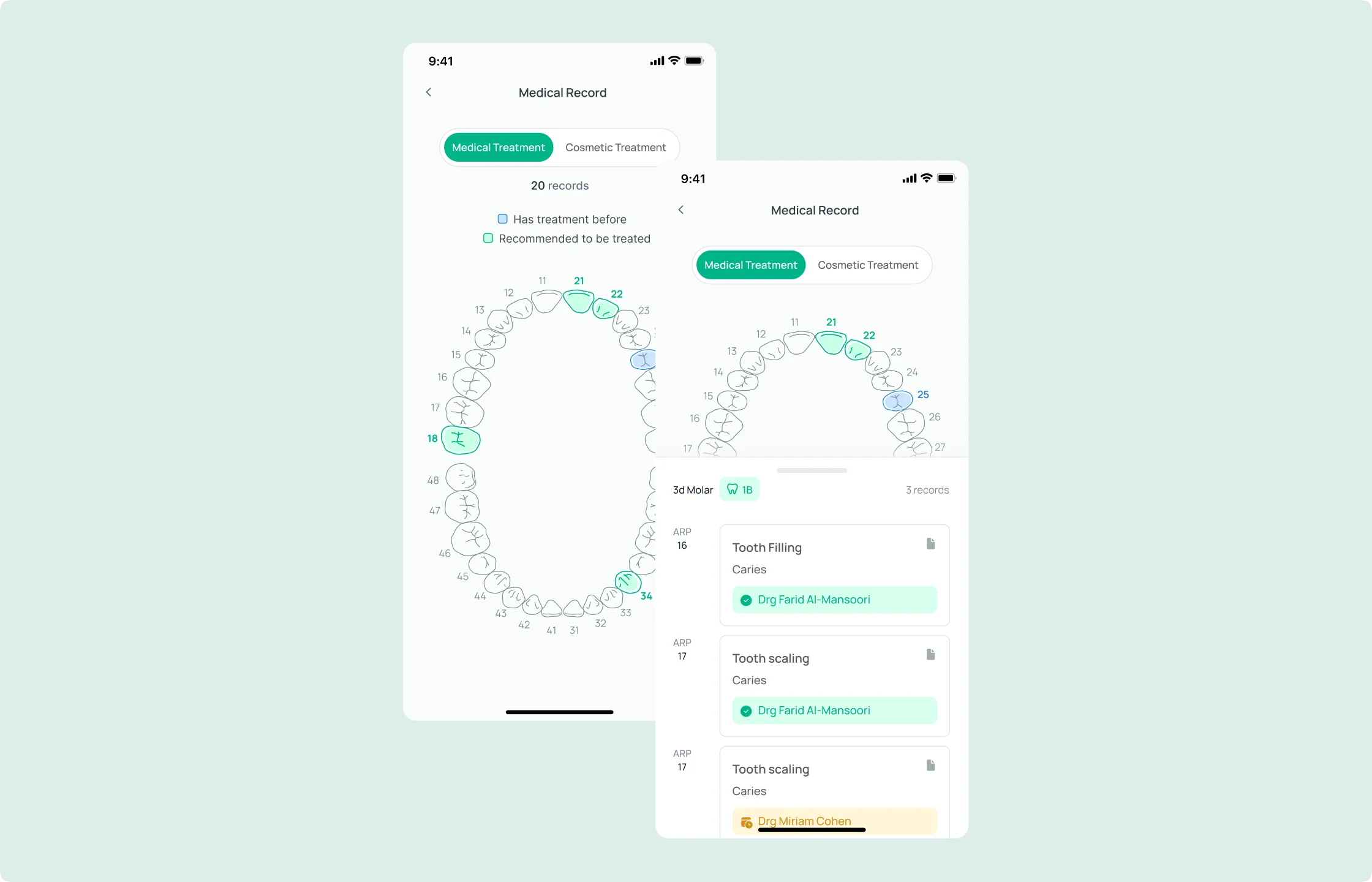
Unified patient medical records
Automation of clinical workflows
Clinical decision support systems (CDSS)
Secure data exchange and interoperability
Integration with telemedicine and remote monitoring
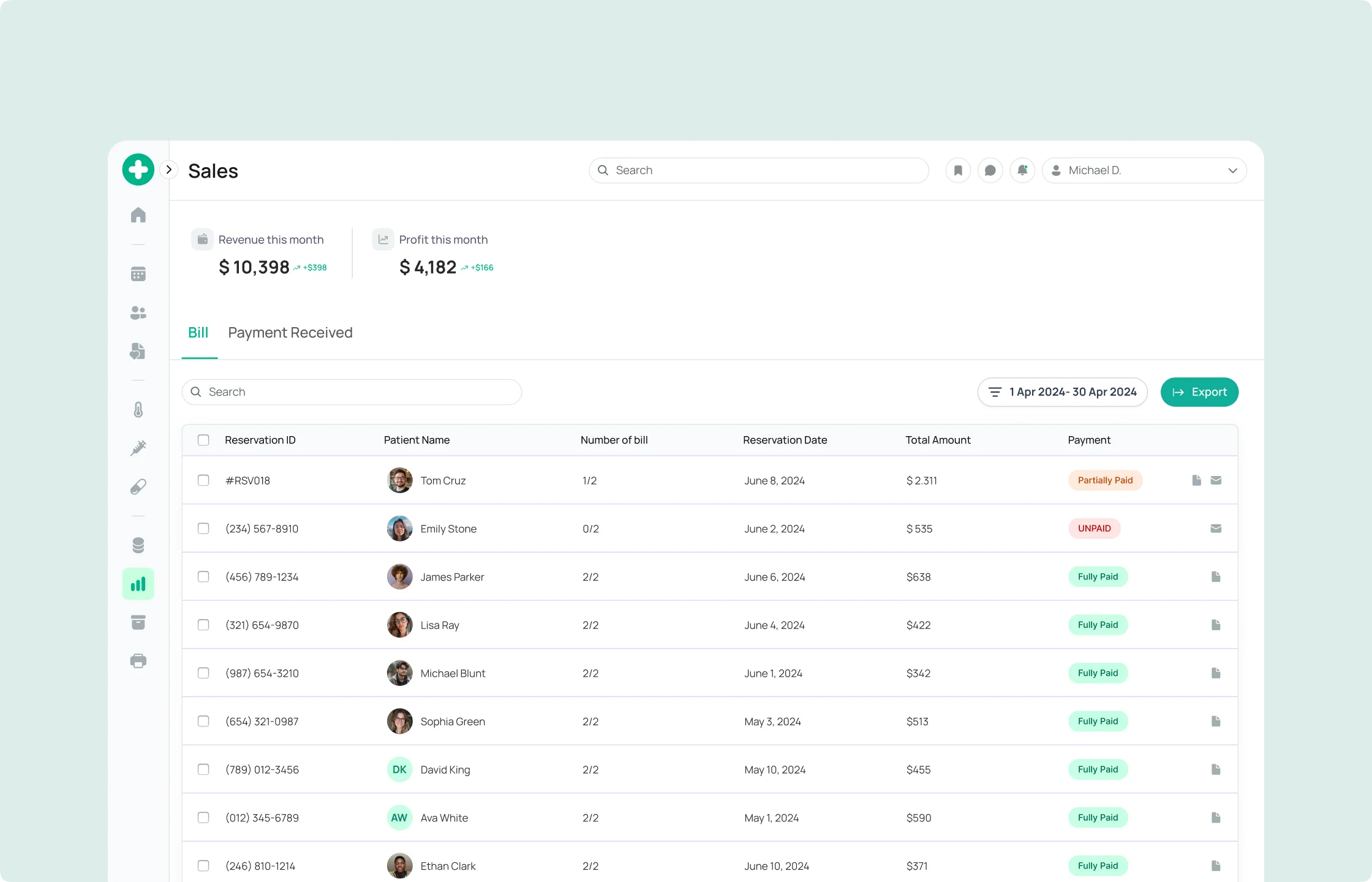
Optimized billing and revenue cycle management (RCM)
User-friendly and secure patient portal
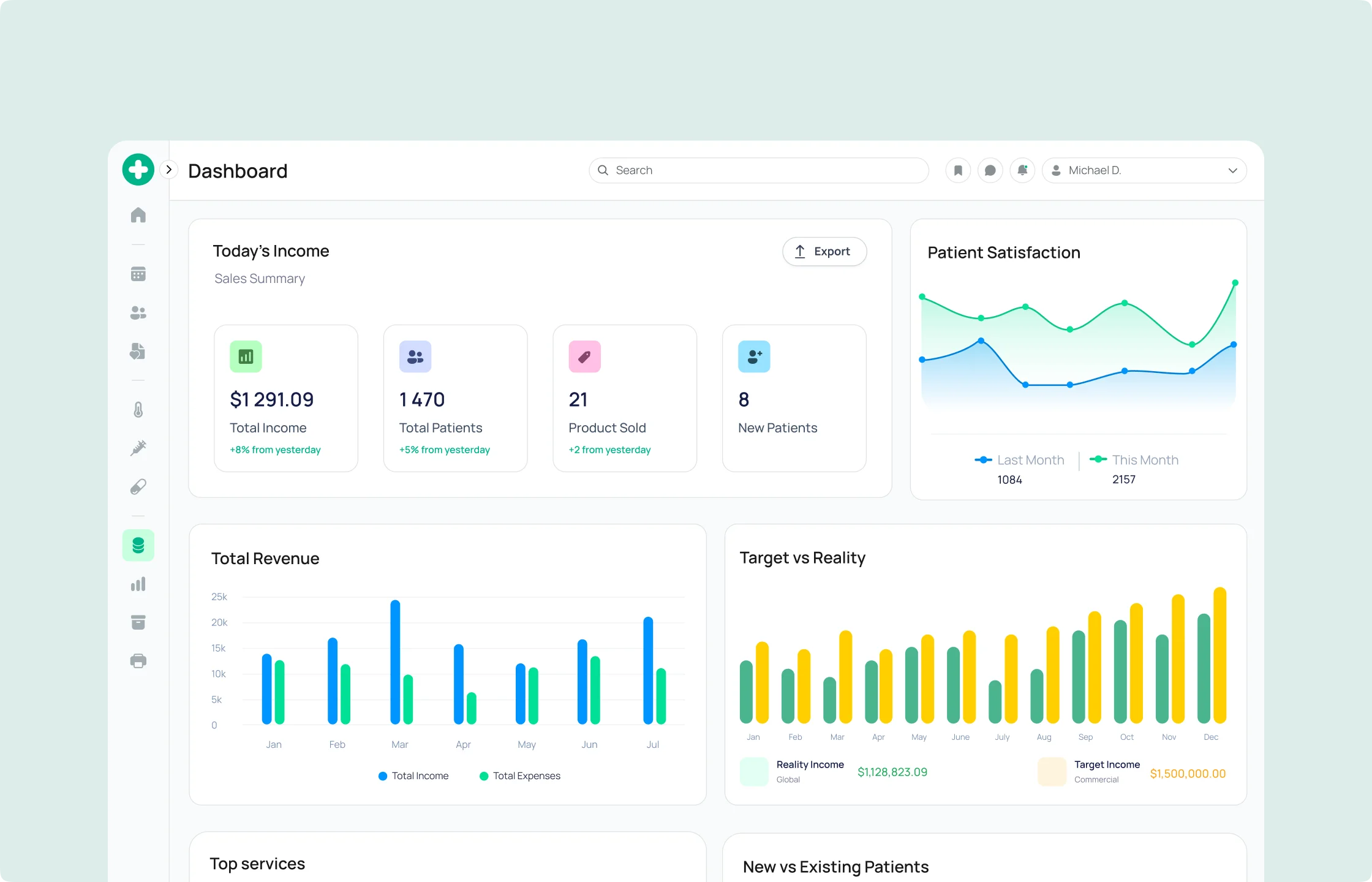
Advanced reporting and analytics for improved care quality
Technology Stack
The solution is built on a highly reliable, scalable, and secure Microsoft Azure technology stack, compliant with the strictest US healthcare regulatory standards:
Results
The implementation of the custom EHR solution led to fundamental changes in the hospital network's operations, directly improving the quality and safety of patient care, as well as optimizing operational processes.
Total annual savings and additional revenue due to Emerline's Custom EHR exceeded $20 million annually. These financial estimates are based on a detailed, third-party verified analysis of the client's operational expenses before and after implementation, as well as comparisons with industry benchmarks for similar improvements. All figures represent the cumulative benefit from various optimizations and do not contain double counting.
- 25% reduction in administrative costs
Automation of routine tasks (scheduling, data entry, billing) significantly reduced staff workload, freeing up resources for more critical tasks. This led to savings of up to $15 million annually in operational expenses.
Before implementation, up to 1/3 of working time was spent on administrative tasks. A 25% reduction in this burden allowed for resource reallocation and avoided hiring additional staff, estimated at millions of dollars for a network of this scale.
- 15% faster diagnosis time
Instant access to unified patient data and CDSS support enabled physicians to diagnose conditions faster and more accurately, reducing waiting times and improving outcomes. This led to increased clinic and hospital throughput, boosting potential revenue by $2-4 million annually by serving more patients and facilitating quicker discharges.
- 35% improvement in data accuracy and completeness
Centralization and automation of data collection, along with built-in validation checks, significantly reduced errors and ensured the reliability of medical records. This led to an 8-10% reduction in insurance claim denials and a decrease in operational losses by $4-6 million annually, directly impacting financial performance.
- Enhanced patient safety and improved clinical outcomes
The implementation of CDSS and reduction in medical errors led to a 15% decrease in serious incidents (e.g., related to medication errors or untimely diagnosis of critical conditions). This contributed to safer treatment and a 5-7% reduction in readmissions (from a baseline of 18% to 11-13%), which is a direct indicator of improved care quality, resulting in savings of up to $1.5 million annually due to reduced compensation and expenses for additional treatment.
- Full compliance with HIPAA, HITECH Act, Meaningful Use, and MIPS regulatory requirements
Implemented security measures and automated reporting ensured 100% compliance, minimizing the risk of fines. This prevented potential penalties that could reach $500,000 - $1 million per incident in case of a serious violation.
- 12% increase in medical staff productivity
Reduced manual work and optimized workflows allowed doctors and nurses to dedicate more time to patients. This led to increased staff efficiency, equivalent to savings of up to $0.7 million annually on overtime or hiring, as well as increased staff loyalty.
- 20% increase in patient satisfaction
Improved access to information through the portal, simplified appointment scheduling, and telemedicine options enhanced patient engagement and their overall experience with service quality. Patient satisfaction surveys showed an average 20-point increase in the Net Promoter Score (NPS) (from a baseline of +30 to +50) within a year of implementation. High patient satisfaction is a key factor in increasing repeat visits and attracting new patients, estimated at $0.3-0.8 million in additional revenue annually.
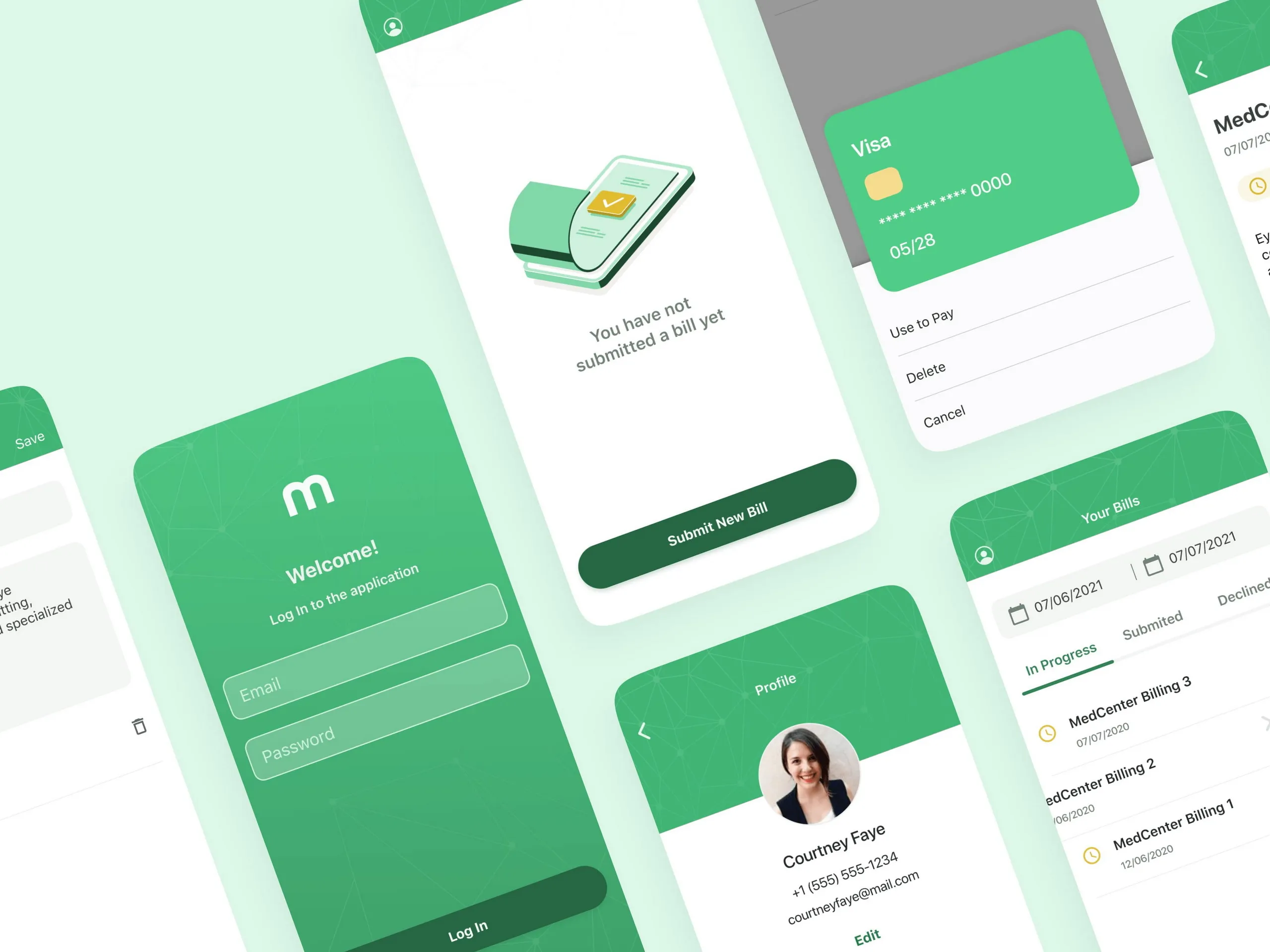
Emerline developed iOS and Android apps to help their customers reach a broader audience of clients, while complementing its web solution with mobile alternatives.
Advanced AI-powered iOS Application Integrated with Innovative Health Tech Software Platform